Don’t Guess, Assess!
Using S-RBD Antibody Tests to Evaluate COVID-19 Immune & Vaccine Responses.

Serological COVID-19 spike protein antibody testing can identify individuals who have been exposed to the SARS-CoV-2 virus, regardless of symptom presentation, and quantify their personal immune response. We offer two testing options for the S-RBD antibody (spike protein receptor binding domain), the target of current COVID-19 vaccines due to the S-RBD antibodies ability to block the passage of COVID-19 to cells. The tests are optimized for pre and post vaccination testing, to deliver the information your patients need based on their individual circumstances.
When combined into a pre/post vaccination assessment, the COVID-19 Immune Response Panel and the COVID-19 Vaccine Response Screen provide clarity into not only when an individual should receive a vaccine, but the effectiveness of their body’s immune response to the inoculation.
What are S-RBD antibodies?
S-RBD stands for “spike protein receptor-binding domain.” The COVID-19 S-RBD binds to the ACE2 receptor and allows the virus access to the body’s cells. Higher levels of S-RBD antibodies have been shown to block or “neutralize” the COVID-19 virus from getting into cells and causing infection.
Typically, Individuals who have recovered from a COVID-19 viral infection usually have high levels of antibodies specific to S-RBD. The “neutralizing” ability of S-RBD antibodies is why all three of the Emergency Use Authorized (EUA) vaccines target the S-RBD, although they use different methods for getting the S-RBD protein information into the body.
Why measure S-RBD antibodies separately?
While human studies indicate that spike protein and nucleocapsid protein antibodies elevate in response to COVID-19 virus exposure, these antibodies are not as specific as the S-RBD antibodies for preventing COVID-19 infection (or re-infection) or for confirming post-vaccination status. After the virus infects the human body, it creates a large quantity of both “neutralizing” antibodies such as S-RBD and many nonspecific endogenous antibodies.
Although a general trend of post-infection increases in spike and nucleocapsid antibodies in association with increased S-RBD antibodies has been observed, measurement of the generalized antibodies is not always predictive of S-RBD status, particularly when the only stimulus is an S-RBD vaccine:

Why measure baseline and post-vaccine responses?
There are several good reasons to measure antibody status before and after a COVID-19 vaccination. Pre/post-vaccination assessment is the only way to be sure that a COVID-19 vaccination was effective. First, not everyone can mount an adequate antibody response to either COVID-19 infection or vaccination, and it is important to protect those that cannot make the needed antibodies.
Second, not everyone needs to be vaccinated immediately. Individuals with natural antibodies from a COVID-19 infection do not require immediate vaccination. After infection, a vaccination only becomes necessary when natural antibody levels begin to drop 3-6 months later. Serial testing can help determine when it’s the right time to vaccinate.
Finally, it is important to assess infection status prior to vaccination because the current Centers for Disease Control (CDC) guidelines advise against vaccination during an active COVID-19 infection. For this reason, two separate profiles are offered for the S-RBD antibody test: the COVID-19 Immune Response Panel and the COVID-19 Vaccine Response screen.
In essence, the best way to ensure your patients’ safety is by not assuming they are protected but rather assessing their status pre and post-vaccination to be certain. These two new testing options are valuable tools to confirm they have reached adequate protection from future COVID-19 exposures.
The COVID-19 Immune Response Panel measures both nucleocapsid (N-protein) and S-RBD antibodies. N-protein antibodies do not rise in response to COVID-19 S-RBD vaccinations. The combined serum IgM/IgG tests measure the body’s response to COVID-19 nucleocapsid (N) and spike protein receptor-binding domain (S-RBD) exposure. The N and S-RBD antibodies’ combination assay has a > 99% positive and negative predictive value 15 days after COVID-19 exposure. This test does not differentiate between IgM and IgG; studies indicate that joint testing is as or more reliable than individual IgM and IgG testing in confirming COVID-19 exposure.

The COVID-19 Vaccine Response Screen measures only the antibody response to the S-RBD protein. Once the baseline immune response has been established, this test can be used post-vaccination to evaluate immune status. The average time for seroconversion has been estimated at 2-3 weeks. However, the strongest antibody responses will likely be seen after the second vaccine dose 6-8 weeks after the first inoculation.

Assess Patient Vulnerability to COVID-19

Advanced Chemiluminescence Technology

95% of Results Available in 24 hours
Testing Process
Each test is performed using a Roche enzyme-amplified chemiluminescence platform (CLA) to detect even exceptionally small amounts of SARS-CoV-2 antibodies. The CLA technique features higher sensitivity than conventional ELISA or rapid lateral flow tests and was purposely selected based on the 30+ years of experience in immunoassay development of our laboratory partner. We are confident this process provides the most accurate results.
These tests are FDA authorized for emergency use.


Specimen Collection
Sample Reports
The reports are straightforward and easy to read, so you and your patient can focus on follow-up care. The reports for the COVID-19 Spike Protein Antibody tests clearly indicate if S-RBD antibodies are present and, when tested for, indicates whether IgG and IgM levels are reactive. The reports also include important information about the test.

Frequently Asked Questions
How long does it take to get test results?
Once the specimen has been received by the lab, you can expect test results in 24-48 hours. 99% of results are available in 24 hours and 5% in 48 hours. You will be able to view the results via our online portal.
Do these tests indicate an active COVID-19 infection?
Antibody tests are not considered diagnostic for COVID-19. The COVID-19 Immune Response Panel measures IgM antibodies which can rise during an active infection.
If an individual is symptomatic or has been recently exposed to COVID-19 we suggest following up with a molecular diagnostic assay to rule out infection in these individuals.
Are these tests FDA-approved?
The COVID-19 Immune Response Panel and COVID-19 Vaccination Response Screen have been FDA-authorized for emergency use.
What are the sensitivity and specificity of these tests?
State-of-the-art, highly sensitive chemiluminescent platforms are used to run these tests. These machines are developed and manufactured in the US and offer the most accurate IgM and IgG coronavirus antibody testing currently available.
The COVID-19 Immune Response Panel has an overall specificity of 99.8% and a sensitivity of 100% at >14 days post-infection.
Can these tests be combined with the COVID-19 Diagnostic Test?
Yes. Consider combining the COVID-19 antibody and diagnostic tests if:
- Swab collection is difficult
- There is a history of COVID-19 symptoms, but subsequent recovery
- You have concerns about a patient’s ability to mount an immune response to the virus
Can these tests be used for children?
There is evidence that this type of test is not as accurate for children. We do not recommend using these tests for children under the age of 2, or children of any age that are currently breastfeeding.
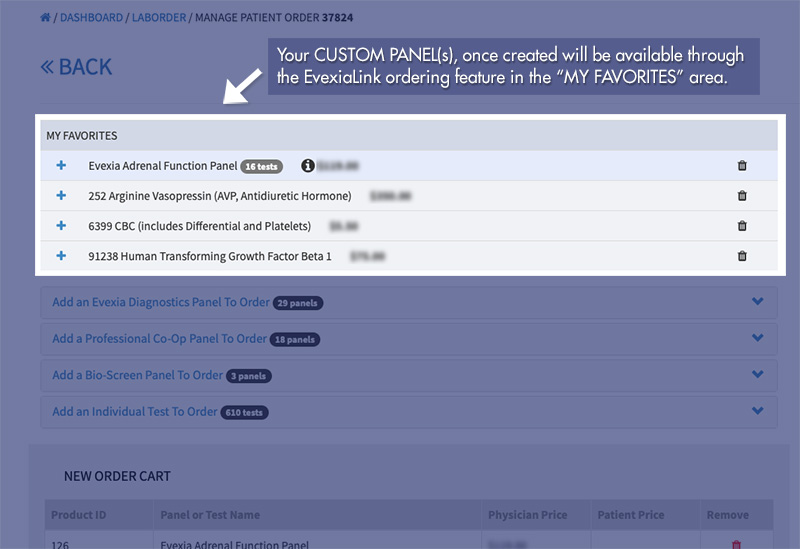
To Order COVID-19 Antibody Tests
References:
Centers for Disease Control and Prevention
(25 Jan 2021) Frequently Asked Questions about COVID-19 Vaccination. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/faq.html#:~:text=The%20protection%20someone%20gains%20from,new%20evidence%20becomes%20available Accessed 12 Feb 2021.
(03 Feb 2021) Myths and Facts about COVID-19 Vaccines. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/facts.html Accessed 12 Feb 2021.
(07 Jan 2021) COVID-19 Vaccine FAQs for Healthcare Professionals. https://www.cdc.gov/vaccines/covid-19/hcp/faq.html Accessed 12 Feb 2021.
Germain N, Herwegh S, Hatzfeld AS, Bocket L, Prévost B, Danzé PM, Marchetti P. Retrospective study of COVID-19 seroprevalence among tissue donors at the onset of the outbreak before implementation of strict lockdown measures in France. Cell Tissue Bank. 2021 Feb 1. doi: 10.1007/s10561-021-09901-3.
Griffin S. (30 Dec 2020) COVID-19: Antibodies protect against reinfection for at least six months, study finds. BMJ 2020;371:m4961
Hall V, et al. Do antibody positive healthcare workers have lower SARS-CoV-2 infection rates than antibody negative healthcare workers? Large multi-centre prospective cohort study (the SIREN study), England: June to November 2020. medRxiv 2021.01.13.21249642; doi: https://doi.org/10.1101/2021.01.13.21249642 Accessed 12 Feb 2021.
Kim TH, Johnstone J, Loeb M. Vaccine herd effect. Scand J Infect Dis. 2011 Sep;43(9):683-9.
Ledford H. (14 Jan 2021) COVID reinfections are unusual — but could still help the virus to spread. Nature. https://www.nature.com/articles/d41586-021-00071-6#correction-0 Accessed 12 Feb 2021.
Moore JP, Offit PA. (2021) SARS-CoV-2 Vaccines and the Growing Threat of Viral Variants. JAMA. doi:10.1001/jama.2021.1114 Accessed 01 Mar 21 https://jamanetwork.com/journals/jama/fullarticle/2776039
Premkumar L, et al. The receptor binding domain of the viral spike protein is an immunodominant and highly specific target of antibodies in SARS-CoV-2 patients. Sci Immunol. 2020 Jun 11;5(48):eabc8413.
Sampath Kumar NS, Chintagunta AD, Jeevan Kumar SP, Roy S, Kumar M. Immunotherapeutics for Covid-19 and post vaccination surveillance. 3 Biotech. 2020 Dec;10(12):527. doi: 10.1007/s13205-020-02522-9.
Sewell H. (17 Dec 2020) Covid-19 vaccines: delivering protective immunity. BMJ 2020; 371 doi: https://doi.org/10.1136/bmj.m4838 Accessed 12 Feb 2021.
Zhou Z, Wang X, Fu Y, Zhang X, Liu C. Letter to the editor: Neutralizing antibodies for the treatment of COVID-19. Acta Pharm Sin B. 2021 Jan;11(1):304-307.